Venous thromboembolic (VTE) disease, the syndrome in which blood clots form in the deep veins and often break loose to travel to the lungs, is one of the most difficult and serious problems in modern medicine. Early recognition and appropriate treatment of deep venous thrombosis (DVT) and pulmonary thromboembolism (PTE) can save many lives.
Problem: DVT causes morbidity and mortality both by its behavior in the deep veins and by embolization to the lungs and other parts of the circulation. Because DVT and pulmonary embolism (PE) are a single disease, it is misleading to consider the two conditions separately. Prospective studies in patients with proven DVT but without any signs or symptoms to suggest PE find that roughly half of these "asymptomatic" patients have experienced undiagnosed PE. The more precise the test, the more it appears that virtually every case of DVT embolizes to some extent. With or without PE, DVT itself may be occult. Two thirds of patients with proven PE have no DVT symptoms, and one third of the time it is impossible to find the original site of DVT without an autopsy.
All currently available diagnostic tests for DVT are more sensitive and more specific when a patient has lower extremity pain and swelling than when a patient has asymptomatic DVT. All are likely to miss thrombus below the knee or above the groin and are less sensitive for the detection of nonobstructing thrombus than for obstructing thrombus.
Frequency: The true prevalence of VTE in the population at large generally is underestimated because most studies depend on the recognition of clinically apparent disease. This approach fails for VTE because many cases are clinically inapparent and because many clinically apparent cases are misdiagnosed. The problem is compounded in retrospective studies, in which incomplete chart notes and inaccurate recollection further cloud clinical certainty.
The best epidemiological evidence today comes from the 30-year prospective study of men born in 1913. For every 100,000 person-years, this study found an incidence of 387 cases of recognized venous thrombosis, of which 285 subjects had a diagnosis of PE and 107 had fatal PE. This corresponds to an average of 39 cases and 11 deaths per year in a practice of 10,000 patients. One of every 9 persons develops recognized DVT when younger than 80 years, and clinically recognized VTE accounts for 1 of every 20 deaths in those older than 50 years. Autopsy studies demonstrate that approximately 80% of all cases of DVT and PE remain undiagnosed, even when they are the immediate cause of death. Therefore, the true prevalence in the population at large is probably much higher.
Although the prevalence of DVT and PE is highest in patients hospitalized and at bed rest with serious coexisting illnesses, the prevalence in ambulatory outpatients is not insignificant. Emergency department patients whose symptoms include pleuritic chest pain have a rate of PE of 21%.
Etiology: A clinical suspicion of DVT or PE often stimulates efforts to identify known risk factors for venous thrombosis. All recognized risk factors for DVT (and thus for PE) arise from the 3 underlying components of the Virchow triad: venous stasis, hypercoagulability, and vessel intimal injury. Although the presence of known risk factors increases the likelihood of PE, the opposite is not true because the absence of occult risk factors cannot be confirmed without an extensive workup.
The single most powerful risk marker for DVT is a prior history of VTE. In the absence of prophylaxis, patients who have had prior recognized PE or extensive DVT are virtually certain to develop recurrent VTE with surgery. An increased risk of DVT is also recognized in clinical settings such as the postoperative period, pregnancy, and the puerperium. DVT is common in patients with local trauma and stasis, such as that associated with a leg cast, and in those who smoke, are obese, or travel in confined circumstances (the so-called coach-class syndrome). Other clinical settings commonly reported as risk factors for venous thrombosis are reviewed here.
Anesthesia
Patients receiving general anesthesia have a 500% increased risk of DVT compared with patients receiving epidural anesthesia for the same surgical procedure.
Autoimmune disease and immune deficiency
Of patients with systemic lupus erythematosus, 9% develop spontaneous DVT. The lupus anticoagulant responsible for the excess risk is observed in persons with AIDS and in those with many other autoimmune diseases besides lupus and may be induced in healthy patients by phenothiazine drugs.
Blood surface antigens
Type A blood is associated with lower levels of antithrombin III and higher levels of factor VIII than type O blood. Women of reproductive age with type A blood are 4 times as likely to develop DVT compared with women with type O blood. This association of risk with blood type A does not extend to older men or to women past reproductive age.
Cancer
Malignancy is an important risk factor for DVT, and spontaneous DVT without an obvious cause is an important marker for possible occult malignancy. In 38% of cases of concomitant cancer and DVT, the DVT is detected first. The relative risk for cancer is 19 times higher for patients younger than 50 years who have had DVT than for those without a history of DVT. Fully 16% of patients with angiographically proven PE are diagnosed with cancer within 2 years.
Strokes and neurotrauma
DVT is common after stroke or neurological trauma. Without prophylaxis, half the patients develop acute DVT within 5 days following a stroke. Head trauma may cause defibrination, disseminated intravascular coagulation, and DVT. Forty percent of postoperative neurosurgical patients develop DVT. Stroke patients with a single paretic leg develop DVT in 60% of the paralyzed legs but in only 7% of the nonparalyzed ones.
Chemotherapy
Many types of chemotherapy increase the risk of DVT and PE. Some agents reduce the levels of circulating anticoagulants such as antithrombin III or protein C or S, some cause an increase in circulating procoagulants such as von Willebrand factor, and some depress fibrinolytic activity.
Coagulopathy
Deficiencies of protein C, protein S, or antithrombin III are well-recognized coagulopathies that together account for approximately 15% of the cases of DVT. Resistance to activated protein C accounts for many more. The lupus anticoagulant is another common coagulopathy that can be inherited or acquired.
Patients with familial deficiency of protein C or protein S often experience multiple episodes of DVT or PTE when younger than 35 years. Cancer, chemotherapy, vitamin K deficiency, oral anticoagulant use, surgery, and disseminated intravascular coagulation can trigger an acquired deficiency of protein C.
Antithrombin III deficiency may be familial or acquired. Most cases occur in patients with severe liver disease. If antithrombin III levels are reduced to half the normal circulating level, the patient is at high risk for venous thrombosis. More than half the persons with this deficiency experience PTE when younger than 50 years.
The most important coagulation abnormality remained completely unrecognized until 1995, when Ridker described a resistance to activated protein C that results from a single point mutation in factor V. This newly recognized hypercoagulable state, known as APC resistance or factor V Leiden, is present in 7% of the general population and is responsible for half the cases of DVT that were previously considered idiopathic. In current practice, any reference laboratory can perform the biological assay for APC resistance, and most can also perform the more accurate DNA test for factor V Leiden.
Fibrinolysis
Impaired fibrinolysis occurs in several inherited syndromes but is most common in postoperative patients, those taking synthetic estrogens of any type, and women who are pregnant or status postpartum.
Heart disease
Acute myocardial infarction and congestive heart failure increase the likelihood of DVT and PE, independent of bed rest or immobilization. Patients with acute myocardial infarction who are not receiving anticoagulation have a 26-38% rate of DVT, while similar patients treated for acute myocardial infarction but in whom infarction is eventually excluded have a much lower rate of DVT.
Hyperlipidemia
The presence of lipemic serum greatly increases the rapidity and extent of thrombus formation in response to vascular injury.
Immobility
Immobilization that produces stasis is the most important risk factor for DVT and PE. Hospitalized patients should be kept ambulatory whenever possible because DVT occurs in 10% of all patients placed at bed rest in a general medical ward and in 29% of those placed at bed rest in an intensive care unit. Unsuspected PE is a common contributing cause of death in all types of disease. Autopsy findings from patients dying in the hospital from any cause demonstrate PE in 15% of those dying after less than 1 week in the hospital and in 80% of those who die after more prolonged periods of immobilization.
Increasing age
Increasing age leads to an increased risk of DVT and PE, although whether this is entirely independent of associated factors such as other underlying illness and immobility remains unknown.
Inflammatory bowel disease
Patients with ulcerative colitis or Crohn disease are at increased risk for DVT and PE because of increased fibrinogen, factor VIII, and platelet activity and depressed levels of antithrombin III and alpha2-macroglobulin.
Miscellaneous
Homocystinuria and the Shwartzman reaction (ie, immunologic generalized thrombosis) both increase the risk of thromboembolism.
Obesity
Obesity (weight >20% above ideal weight) has long been accepted as a risk factor for DVT and PE, but the evidence supporting this association is not convincing. When associated factors such as history, illness, immobility, and age are taken into account, obesity may not truly be an independent risk factor.
Oral estrogens
No published prospective randomized studies have definitively tested and compared the prevalence of DVT or PE in patients taking or not taking oral contraceptives. Case-control and cohort studies based on clinical signs and symptoms of thrombosis suggest a relative risk of approximately 3-12 times higher for patients taking oral contraceptives compared with those not taking them.
Polycythemia and thrombocytosis
The risk of venous and arterial thrombosis increases linearly with an increasing hematocrit value. Forty percent of deaths in patients with polycythemia vera are related to thrombosis, but only a third of these are due to venous thrombosis. Thrombocytosis may increase or decrease the risk of thrombosis depending on the clinical setting, but platelet counts greater than 1 million most often reduce the likelihood of thrombosis and increase the likelihood of bleeding problems.
Pregnancy and puerperium
PE is the most common nontraumatic cause of maternal death in pregnancy, and the prevalence is even higher in the postpartum period. In Sweden, 53 peripartum maternal deaths occurred between 1971 and 1980, and 10 of these were due to PTE. Published reports of the incidence of DVT in postpartum patients ranges from 0.61-20 cases per 1000 peripartum months.
Prior DVT
Patients with a prior episode of DVT are 5 times more likely to develop new DVT compared with patients with no prior episodes of DVT. Prior DVT increases the risk of new postoperative DVT from 26% to 68%. A history of prior clinically apparent PE increases the risk of new postoperative DVT to nearly 100%.
Surgery
Perioperative DVT can result from minimal venous endothelial injury. The rate of postoperative DVT in patients who do not receive effective prophylaxis is 70% after nonelective hip surgery, 48% percent after elective orthopedic surgery, and 12% after elective general surgery. Approximately one fifth of the cases of postoperative DVT cause a clinically apparent PE, and approximately one third of these are fatal. Even when prophylactic heparin is used, 5-10% of postoperative orthopedic patients develop PE. Nearly half of all deaths in orthopedic surgery patients are due to PE.
Tissue antigens
HLA antigens Cw4, Cw5, and Cw6 are associated with an increased frequency of DVT and PE.
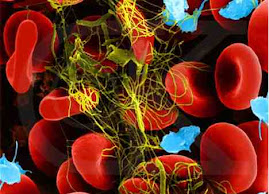
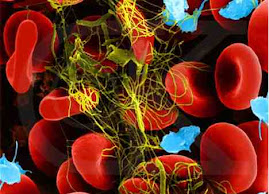
Pathophysiology: Millions of tiny injuries occur within normal blood vessels each day, and millions of tiny microthrombi are formed and lysed in a dynamic balance of functional hemostasis without clinically apparent venous or arterial thrombosis. The German pathologist Virchow demonstrated in 1846 that flow stasis, altered coagulability, or extensive vessel wall injury may cause microthrombi to propagate, resulting in macroscopic thrombi. Vessel wall endothelial damage is the most important of these 3 factors because even minor endothelial injury often results in an accumulation of macroscopic thrombi in the veins.
In a sense, thrombus formation at the site of injury is like normal cicatrization of a dermal wound. In a patient with increased coagulation or defective anticoagulation, thrombus formation can be overly exuberant, similar to the formation of a hypertrophic scar. If fibrinolysis is inhibited, the thrombus extends away from the area of the original vascular injury to invade areas of normal endothelium, similarly to keloid formation. Disorders of hemostasis, coagulation, anticoagulation, or fibrinolysis occur in a variety of clinical settings that can cause recurrent DVT or PE and premature arteriosclerotic syndromes or myocardial infarction at an early age.
Hemostasis
The initiating event in venous thrombosis is platelet adhesion. Even minimal vascular endothelial injury reliably initiates a predictable sequence of events that results in platelet adhesion and thrombus formation. Initial platelet adhesion and aggregation are stimulated by a component of endothelial cells, most likely a substance known as amorphous electron-dense substance, which is exposed by endothelial cell injury. The release of this substance is enhanced by activity of the intrinsic coagulation cascade and is inhibited by platelet antiaggregating agents, thrombolytics, and anticoagulants.
Platelet activation causes the release of platelet proaggregants thromboxane A2 and serotonin, resulting in the aggressive recruitment of more circulating platelets to form a hemostatic plug. Thromboxane A2 and serotonin also act to bring about local vasoconstriction. Exposed platelet membrane phospholipids catalyze the activation of factor X and the local (endothelial) formation of thrombin, itself a powerful proaggregant. Thrombin-mediated platelet aggregation is unaffected by aspirin and nonsteroidal anti-inflammatory agents, but aggregation caused by platelet-derived thromboxane A2 is dependent on platelet cyclooxygenase, which is reversibly inhibited by nonsteroidal anti-inflammatory agents and is irreversibly inhibited by aspirin.
Coagulation
After a hemostatic plug is well established, coagulation pathways are activated and thrombin is generated. Fibrin cross-linking builds a true thrombus out of what was initially a loose aggregation of blood elements. If this series of events were unopposed, any small vascular endothelial injury would result in thrombus propagation throughout the venous system. Three factors serve to retard and prevent uncontrolled propagation: flow dilution, natural anticoagulants, and natural thrombolytics. If blood flow is reduced, activated coagulation factors will accumulate rather than be carried away. If this happens or if some defect is present in the production or function of the natural anticoagulants or thrombolytics, the thrombus forms more vigorously than appropriate for a given vascular injury. The patient develops recurrent venous thrombosis and PTE.
Anticoagulation
Protein C, protein S, and antithrombin III are the best understood of the natural circulating anticoagulants. Antithrombin III, which interferes with the action of serine proteases such as thrombin, is a general inhibitor of the intrinsic pathway. Protein C (with its cofactor, protein S) inhibits factor V and factor VIII, principal components of the common coagulation pathway.
Paradoxically, a functional deficiency of the procoagulant factor V increases resistance to the anticoagulant effects of activated protein C. This deficiency is present in nearly half the patients with clinically recognized venous thrombosis. Many other plasma proteins serve as activators, inhibitors, or cofactors in the coagulation cascade, including such known proteases as heparin cofactor II, alpha2-macroglobulin, alpha1-antitrypsin, and C1 inhibitor. Isolated deficiency of heparin cofactor II can cause recurrent venous thrombosis, and other cofactors can increase the likelihood of thrombosis in response to vascular injury or venous stasis. Together, these plasma proteins prevent minor endothelial injury from initiating uncontrolled intravascular coagulation.
Fibrinolysis
Fibrinolysis is the body's defense against the formation of a thrombus. Fibrinolysis is initiated by tissue activators and by circulating activators that transform the inactive precursor plasminogen into the active fibrinolytic agent plasmin. Plasmin attacks and degrades fibrin, and when excess plasmin is present, it also attacks and degrades fibrinogen. Damaged endothelial cells release tissue-type plasminogen activator at the same time they bind platelets and initiate the clotting process. This balancing process ensures that under normal conditions, the formation of a thrombus remains localized to an injured area where it is needed. Any disturbance of the delicate balance leads either to increased bleeding or to increased propagation of thrombi.
The principal physiologic plasminogen activators are urokinase-type plasminogen activator and tissue-type plasminogen activator. The latter is found in the endothelial cells of vein walls and is released in response to physiologic stimuli such as segmental venous stasis, vessel wall injury, exercise, and the presence of thrombin. Most of the action of tissue-type plasminogen activator occurs at the surface of a thrombus, where plasmin is formed after plasminogen and tissue-type plasminogen activator together bind to fibrin. However, circulating tissue-type plasminogen activator produces a systemic lytic state in which circulating fibrinogen is consumed.
Impaired fibrinolytic activity permits thrombus propagation and leads to an increased likelihood of clinically apparent venous thrombosis. Many different problems can interfere with fibrinolysis. Plasminogen levels may be low, or plasminogen may be defective because of structural abnormalities. Fibrinogen and fibrin may be structurally abnormal in such a way as to resist degradation by plasmin. A patient may have high levels of circulating inhibitors of fibrinolysis or low levels of plasminogen activators.
Clinical: The clinical diagnosis of DVT is difficult and fraught with uncertainty. The classic signs and symptoms of DVT are those associated with obstruction to venous drainage and include pain, tenderness, and unilateral leg swelling. Other associated nonspecific findings are warmth, erythema, a palpable cord, pain upon passive dorsiflexion of the foot, and spontaneous maintenance of the relaxed foot in abnormal plantar flexion (the Homan sign). When a patient presents with these symptoms, the diagnosis of venous thrombosis is strongly suggested, but no patient should be treated based on clinical findings alone because even when a patient has a swollen, painful, congested leg that appears to be clinically obvious DVT, the chance that DVT is the correct diagnosis is only 50%.
Conversely, an absence of signs and symptoms does not rule out DVT. Most cases of DVT lack classic signs or symptoms, and thus, DVT is not considered. Only 7% of postoperative renal transplantation patients, for example, display clinical symptoms of DVT, yet prospective investigation leads to the diagnosis in 20% of cases. DVT simply cannot be diagnosed or excluded based on clinical findings; thus, diagnostic tests must be performed whenever the diagnosis of DVT is being considered.
When a patient has DVT, symptoms may be present or absent, unilateral or bilateral, or mild or severe. Thrombus that does not cause a net venous outflow obstruction is often asymptomatic. Thrombus that involves the iliac bifurcation, the pelvic veins, or the vena cava produces leg edema that usually is bilateral rather than unilateral. High partial obstruction often produces mild bilateral edema that is mistaken for the dependent edema of right-sided heart failure, fluid overload, or hepatic or renal insufficiency.
Severe venous congestion produces a clinical appearance that can be indistinguishable from the appearance of cellulitis. Patients with a warm, swollen, tender leg should be evaluated for both cellulitis and DVT because patients with primary DVT often develop a secondary cellulitis, while patients with primary cellulitis often develop a secondary DVT. Superficial thrombophlebitis, likewise, is often associated with clinically inapparent underlying DVT.
If a patient is thought to have PE or has documented PE, the absence of tenderness, erythema, edema, or a palpable cord upon examination of the lower extremities does not rule out thrombophlebitis, nor does it imply a source other than a leg vein. More than two thirds of patients with proven PTE lack any clinically evident phlebitis. Nearly one third of patients with proven PE have no identifiable source of DVT despite a thorough investigation. Autopsy studies suggest that even when the source is clinically inapparent, it lies undetected within the deep venous system of the lower extremity and pelvis in 90% of cases.
DVT below the knee
Although DVT below the knee is widely believed to be benign, this is untrue. Most cases of proximal DVT have their origins in the venous sinuses of the calf, and propagation to the popliteal vein and the femoral vein occurs in 20-30% of cases. However, DVT need not spread proximally to cause fatal PE. The single largest autopsy series ever performed to specifically to look for the source of fatal PE was performed by Havig in 1977, who found that one third of the fatal emboli arose directly from the calf veins.
The lower leg has 3 principal pairs of deep veins: the anterior tibial vein, draining the dorsum of the foot; the posterior tibial vein, draining the sole of the foot; and the peroneal vein, draining the lateral aspect of the foot. DVT that is isolated to the anterior tibial vein results in PTE in 30% of cases and is responsible for many deaths. Other deep vein groups draining the lower leg include the gastrocnemius plexus and the soleal plexus. These plexuses and the deep venous groups named above all drain via the popliteal vein at the knee. Thrombosis of the popliteal vein results in PTE in 66% of cases, a frequency similar to that of DVT in the thigh.
Calf deep vein thrombophlebitis is an important cause of morbidity quite aside from any risk of propagation or of embolization. Isolated calf vein thrombophlebitis results in clinical postphlebitic syndrome in 20-40% of cases. The pathophysiology of the postphlebitic syndrome has been well established as one in which the recanalization of thrombosed deep veins results in the destruction of the venous valves, leading to chronically elevated ambulatory venous pressure within the legs. Valve incompetence need not be extensive to produce venous hypertension and clinical symptoms. Isolated incompetence of the valves in the popliteal segments of the deep venous system leads to elevated ambulatory venous pressures averaging 72 mm Hg, and more than 60% of those with isolated popliteal valve failure develop severe clinical signs of chronic venous insufficiency (CVI). This postphlebitic syndrome is responsible for chronic pain, edema, hyperpigmentation, and ulceration and for many cases of recurrent DVT and PE.